About PCDH19
What is PCDH19 Epilepsy?
PCDH19 Epilepsy is a disease with a wide spectrum of severity in seizures, cognitive delays and other symptoms, which are all caused by a mutation of the PCDH19 gene on the X chromosome.
Please note: This site should not and does not replace medical information or advice from health care professionals.

PCDH19 Genetics
PCDH19 primarily affects females, due to the way the gene is located on the X chromosome. In females, who have two X chromosomes, the presence of one affected and one unaffected copy can lead to a mix of normal and abnormal cells, causing the symptoms of PCDH19 Clustering Epilepsy. Males typically have only one X chromosome, and if it carries the mutation, they are usually asymptomatic. However, males who are mosaic, a rare condition where only some cells carry the mutation. As a result, the condition is much more common and typically more severe in girls, but boys can still be affected in unique and complex ways.
Inheritance
Males with the mutation, who will be largely unaffected, will pass the mutation onto 100% of their daughters and none of their sons. Women with the mutation have a 50% chance of passing it to their daughters and will pass it to 50% of their sons.
Some females who carry the mutation seem to be unaffected, and we still do not understand why. are studying to learn what is protecting them from the disorder. Mosaic males are also affected, but so far very few males have been diagnosed.
Learn More About PCDH19 Genetics
The PCDH19 Alliance created a video series on the genetics of PCDH19. See all videos in the series.
PCDH19 Genetics 1: Understanding Genes & Chromosomes
Learn more about the genes and chromosomes related to PCDH19. This is the first in an ongoing series of instructional...
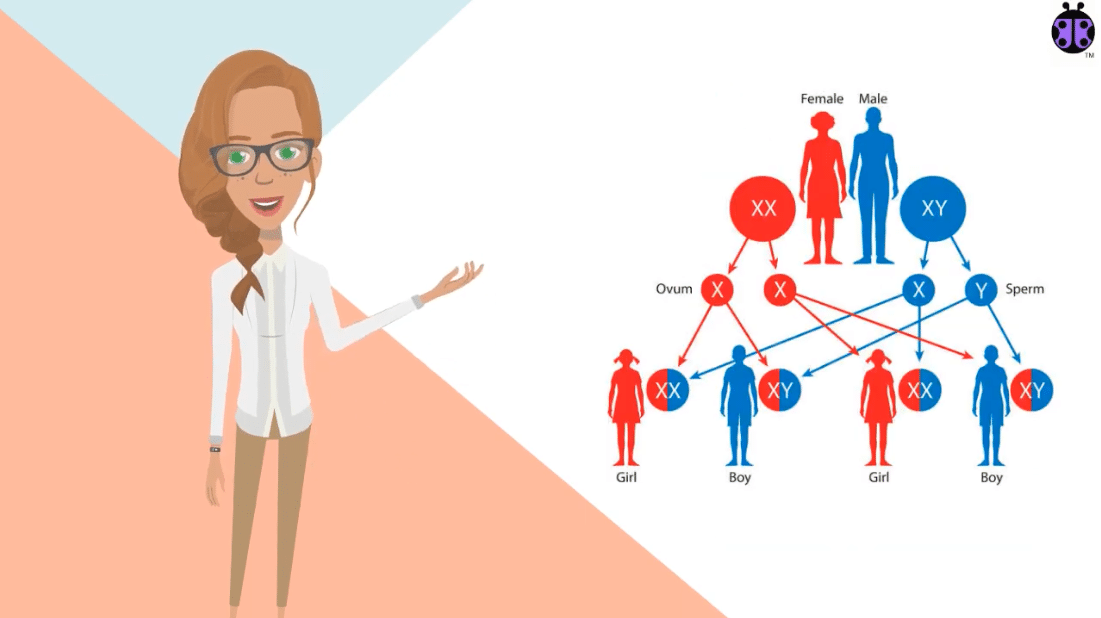
PCDH19 Genetics 2: Inheritance
Learn more about the inheritance of genes related to PCDH19. This is the second in an ongoing series of instructional...
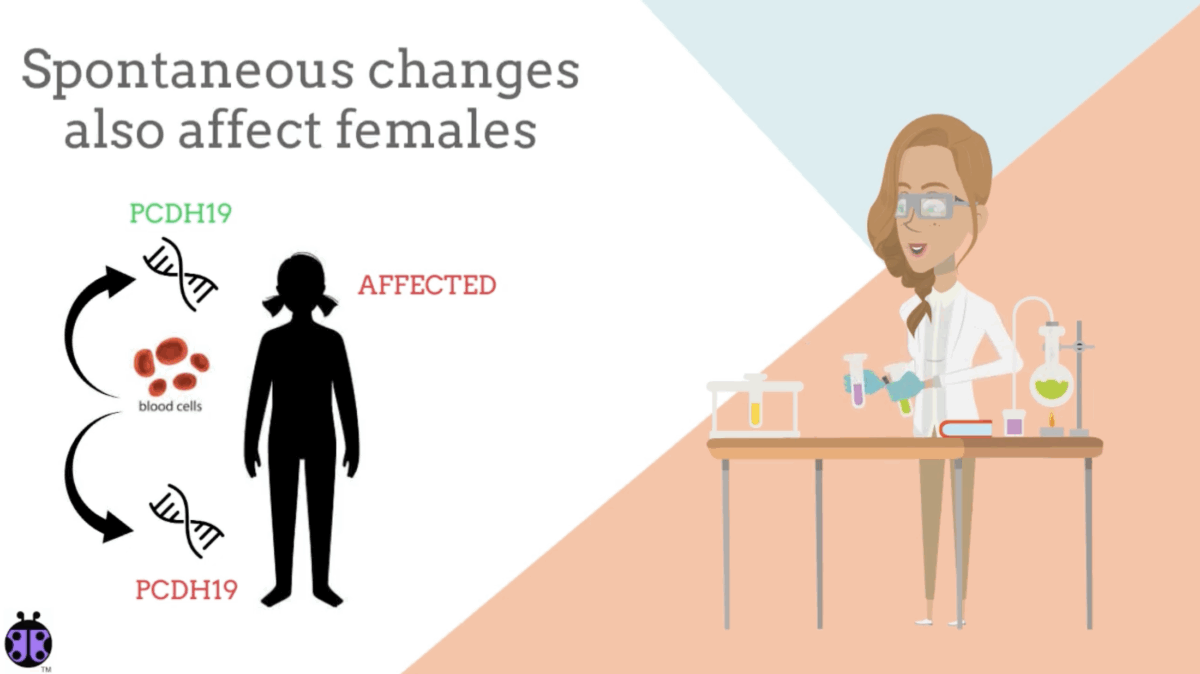
PCDH19 Genetics 3: X-Chromosome Inactivation & Mosaicism
Learn more about the X-chromosome inactivation and Mosaicism related to PCDH19. This is the third in an ongoing series of...
Newly Diagnosed?
If your child has recently been diagnosed with PCDH19 Epilepsy, we’re here to help.
What symptoms are associated with PCDH19 Epilepsy?
Seizure Clusters
The most consistent feature of this disease is seizures that come in clusters and last for days or weeks at a time and do not respond well to available medications.
- The first seizures usually occur between 3 months and 3 years of age with an average of 9 months.
- At first, the seizures usually occur in the setting of a fever, and later they come with no known trigger.
- Sometimes loss of hearing, and loss of skills are experienced after seizure clusters.
- Seizures are often drug resistant and difficult to control.
Seizure Types
The most common seizure types for PCDH19 Epilepsy:
- Generalized tonic-clonic
- Tonic, clonic
- Complex partial
- Atypical absence
- Atonic drop
- Myoclonic seizures
These seizure types may be accompanied by rapid oxygen desaturations and cyanosis.
Cognitive/Intellectual
It is estimated that about 70% of PCDH19 patients have intellectual disability of varying degrees, ranging from mild to severe. The course of development usually follows one of three paths:
- Normal development from infancy, but with regression after seizure onset.
- Normal development and intellectual ability from birth without regression.
- Delayed from birth and remains delayed through adulthood.
Psychiatric
- Autism spectrum disorder or autistic features (estimated at 60%)
- Behavioral problems
- Aggression
- ADD/ADHD
- Anxiety.
- Obsessions (OCD)
In adolescents and adults, depression, bipolar, schizophrenia, psychosis and other mental illnesses have been reported.
Other
- Sleep disturbances, trouble falling and/or staying asleep
- Ictal Apnea – Many individuals also stop breathing during their seizures and have rapid and sometimes prolonged oxygen desaturations.
- Hypotonia (low muscle tone)
- Fine and gross motor deficits
- Language delay or non-verbal
- Sensory integration issues
- Dysautonomia
- Delayed tooth eruption
- Issues with constipation (whether due to disorder or medications)
The Future
What to Expect
Though difficult-to-manage seizures and intellectual disability (ranging from mild to severe) are common in PCDH19 Epilepsy, due to the broad range of clinical manifestations it is impossible to predict what course an individual’s health will take. This is particularly true because the PCDH19 gene was only discovered in 2008.
With newly discovered genetic diseases, typically the more severe cases are discovered first. But as awareness increases in the medical community and genetic testing becomes more widespread, milder phenotypes are often discovered.

Learn More About PCDH19
Browse our resource library to learn more about PCDH19.
Newly Diagnosed
We are here to help you take the first step after a diagnosis with confidence and support.
Parents
We offer resources for parents navigating life with a child or adult with PCDH19 Epilepsy.
Siblings
Siblings of people with PCDH19 Epilepsy deserve support and attention as well.
Self-Advocates
We believe in providing resources to support and empower individuals living with PCDH19 Epilepsy.
The cure is out there. Help us find it.
Your donation brings us one step closer to a cure for PCDH19 epilepsy.

